If you're sexually active, chances are you've probably worried about STIs at some point. Google is often our first port of call when we're in the midst of an STI panic, but in the age of online sex misinformation, that comes with a risk. Getting accurate, reliable information about sexual health on the internet can be a complete minefield.
We talk a lot about the importance of understanding STIs, how they happen, and discussing them with sexual partners so that we can make informed choices regarding our sexual and reproductive health. The most common STI is chlamydia, with the Centre for Disease Control (CDC) declaring it the most reported sexually transmitted infection. It says there were four million chlamydial infections in 2018, and estimates that 1 in 20 sexually active young women aged 14-24 years has chlamydia.
Usually, chlamydia infections develop in the vagina or anus following sex where protection has not been used, but did you know you can get chlamydia in your throat, too?
Want more sex and dating stories in your inbox? Sign up for Mashable's new weekly After Dark newsletter.
A lot of people make the mistake of thinking oral sex is completely STI-proof. Unfortunately, you’re not protected from pesky infections if you’ve had oral sex without using protective barriers like a dental dam. You could contract oral chlamydia.
What is oral chlamydia?
Rebecca Pickerill, clinical practice development manager at Brook, an NHS sexual health services provider, sayschlamydia is a bacterial infection, which can be transmitted through vaginal, anal, and oral sex generally. This means that chlamydia, while mostly considered a vaginal or anal infection, can also appear in and around the mouth.
"Chlamydia is asymptomatic (meaning it has no symptoms, which can make it impossible to spot without an STI test) and it's treated with oral antibiotics," she tells Mashable.
Dr. Rebecca Mawson, resident STI expert at contraceptive review platform The Lowdown says the most common place of infection is in the genitals and caused by penetrative sex. In rare cases it can also affect other parts of the body "like the rectum, throat, and conjunctiva in the eye. Oral chlamydia is probably not quite the right terminology [even though it is commonly used] as it is actually the back of the mouth and throat that is affected."
SEE ALSO: Young men are stressed out about sex, report finds"We don’t really know how commonly women have chlamydia in the throat as most clinics do not routinely screen for it. We tend to do vagina self-screening for chlamydia but not all sites like the rectum and throat," she explains.
However, Pickerill explains that when a person is treated for vaginal chlamydia, after testing positive, the treatment would cover oral chlamydia as well. "The antibiotics given would treat all infection sites, including oral, anal and vaginal chlamydia. In practice, we don't test routinely for oral chlamydia due to test validity but testing is a clinical decision and would be based on an individual case assessment," she explains.
How is oral chlamydia caused and what are the symptoms?
Chlamydia infections in the throat are contracted from oral sex without using condoms or oral dams to prevent infection spreading from genitals to the throat. If a person who has chlamydia has unprotected oral sex without these barriers with another person, they could contract the infection.
SEE ALSO: How to perform cunnilingus like a proMawson notes that chlamydia infections, no matter which body part if infected, are often symptom free. Mawson says "if someone was to have chlamydia in their throat that does have symptoms, they would probably be very similar to a normal sore throat like pain on swallowing and a low grade fever." However, this is rare. Most of the time, chlamydia is asymptomatic.
A common myth about STIs is that you can only catch them once. This is untrue. You can contract chlamydia repeatedly, particularly if you often engage in unprotected sex without the use of barrier protection and are not regularly testing for STIs, which can cause complications.
SEE ALSO: How to give a blowjob like a pro"If you have an infection it is really important to make sure all current sexual partners are treated so that you don’t get re-infections," Mawson explains.
"If you have an infection it is really important to make sure all current sexual partners are treated so that you don’t get re-infections."What to do if you think you have oral chlamydia
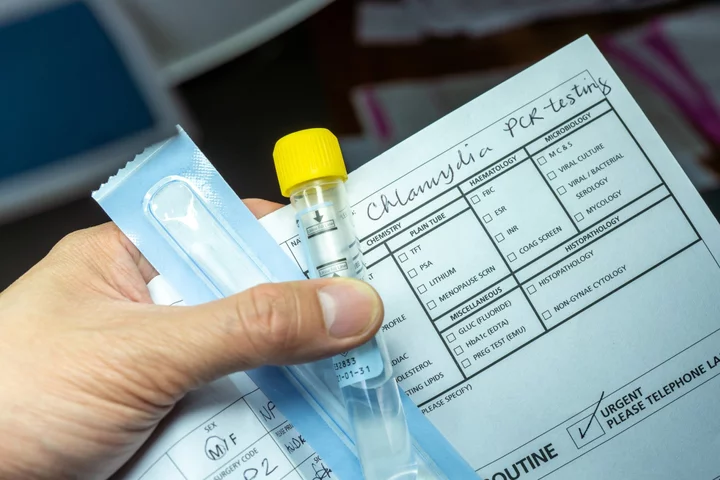
The best place to go if you are worried about oral chlamydia is your local sexual health clinic. They are used to managing infections of all different types and can talk about any concerns you have. Often you can do a an oral swab to see if you have an infection, which you can perform yourself. There are also online services but most only offer a genital screening, as oral screenings are not part of standard routine tests.
As Pickerill explains, normal screening in the UK unfortunately assumes everyone that has oral sex will have had penetrative sex, so individual oral testing is not usual. So, if you only have oral sex it is important to get screened via your local clinic but you might have to discuss with a doctor or nurse first as you won’t fit the usual criteria.
"This is different for men who have sex with men," Mawson adds. "If they give oral sex they are routinely offered a throat swab for chlamydia and gonorrhoea as they have higher rates."
SEE ALSO: Can you take an STI test when you have your period?How to prevent oral chlamydia
To prevent cases of oral chlamydia, it’s important to always get an STI test whenever you start a new relationship or have sex with a new sexual partner. In fact, it’s best if you can both get one done around the same time.
You should also make sure you get an STI test if you have unprotected sex, especially unexpectedly (such as with incidents of condoms breaking/tearing or forgetting to take a contraceptive pill). Mawson says how long you should wait for a test after unprotected sex depends on what you’re screening for. "After unprotected sex wait 2 weeks for chlamydia and gonorrhoea, 4 weeks for syphilis and HIV (in some circumstances you also need a test at 3 months)," she says.
"After unprotected sex wait 2 weeks for chlamydia and gonorrhoea, 4 weeks for syphilis and HIV (in some circumstances you also need a test at 3 months)."Mawson explains that these tests can be done discreetly by ordering online and having them posted out. "If your partner is negative for chlamydia and not having other sexual partners then you won’t get oral chlamydia. If you don’t have a regular partner and you want to protect yourself then use a condom with male partners and oral dams with female partners," she advises.
It’s unfortunate that most sex clinics don’t test for oral infections as part of routine screening, which demonstrates how focused society (and medical professionals) are on penetration as the only ‘real’ type of sex. But oral chlamydia is very much a possibility, and although it’s not part of the typical STI test, don’t let this stop you from seeking medical advice after unprotected oral sex — especially if a sexual partner tells you they’ve tested positive. Visit a sexual health clinic if you have any worries and be open with clinicians. Any good specialist will allow you to take an oral swab if you have any cause for concern.