When Richard Scolyer was diagnosed with a deadly brain tumor in June, he grasped the test results as well as any of his doctors. One of the world’s top cancer pathologists, he gave himself nine months to live at most.
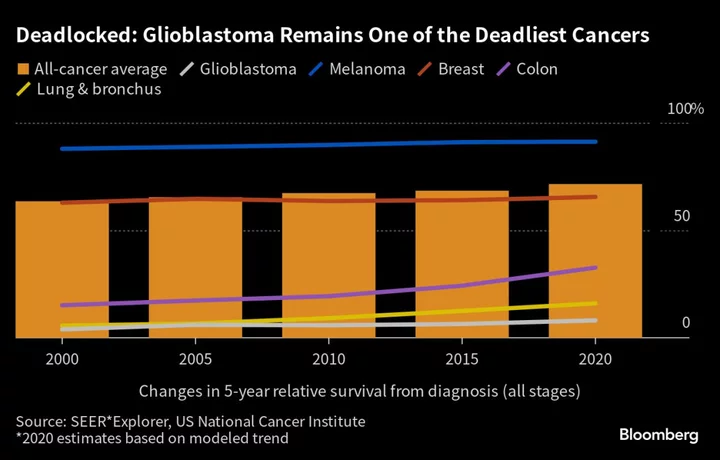
Stage-four glioblastoma multiforme — the most common brain malignancy in adults — is notoriously lethal, even with the best care available. Most of the 14,000 Americans diagnosed each year die within 16 months.
The Australian scientist saw his illness not as a death sentence, but a second opportunity to transform treatment for a stubbornly intractable form of cancer. More than a decade ago, he and his University of Sydney research partner, oncologist Georgina Long, took on a similar challenge, helping to pioneer the use of immunotherapy drugs against melanoma, a form of skin cancer with a reputation as deadly as that of the tumor in his brain.
The powerful medications haven’t performed as well against glioblastoma, and none are approved to treat it. That’s left doctors to depend on the traditional chemotherapy that’s been used for about 20 years with minimal improvement in average survival. But in a world-first for the disease, Scolyer and Long bypassed standard therapy to use a potent cocktail of immune checkpoint inhibitor drugs as initial treatment, followed by another innovative approach — a personalized cancer vaccine.
“Accepting that status quo was never going to be an option,” Scolyer told reporters Sept. 20 at the National Press Club of Australia in Sydney. “I spent my life diagnosing and researching cancer, so why would I stop now?”
It will be months before anyone knows how well the treatment worked, if at all. Pharma companies have tried the new drugs in glioblastoma largely without success, though not in potent combinations like the one Scolyer received. The medications have usually been given after surgery to remove the tumor, which may have impaired the hoped-for immune response. Treating the cancer quickly and repeatedly with immunotherapy drugs may also improve the chances of success.
Scolyer and his colleagues expect to mine new findings from their approach that will help tackle one of the hardest-to-treat cancers. Glioblastoma colonizes the brain like an invasive garden weed, choking off vital healthy tissues. New malignant growths sprout while existing ones branch out with microtubes that can interconnect insidious, drug-resistant cancer cells.
Expanding tumors put pressure on nerves, leading to symptoms ranging from headache to memory and vision loss, difficulty with speech, weakness, seizures and paralysis. While surgery aims to remove the bulk of the main growth, countless microscopic cancer cells often remain in the periphery, relentlessly dividing.
“It’s those tumor cells you can’t see, spreading silently within your brain, that eventually reappear and ultimately prove fatal,” Scolyer said. “To remove my cancer, you’d need to remove a large part of my brain, which is probably not compatible with life.”
Mutation Levels
Tom Parker, a singer for the British-Irish boy band The Wanted, died at age 33 in March 2022, 17 months after he was diagnosed with glioblastoma. Late Massachusetts Senator Ted Kennedy lost his battle at 77, 15 months after his May 2008 diagnosis. President Joe Biden’s eldest son, Beau, received standard treatment in 2013 and returned to work a few months later. The cancer recurred in May 2015, and he died days later at age 46.
Despite results like these, conventional therapy — surgery followed by cell-killing radiation and chemotherapy — hasn’t changed since 2005. Oncologists often refer to certain tumors like glioblastoma as “cold” — lacking the immune response that powers Merck & Co.’s bestseller Keytruda and other checkpoint inhibitors.
Scientists observed decades ago that cancers use certain proteins to cloak themselves from the body’s immune system. Checkpoint inhibitors lift that cloak, enabling cancer-killing T-cells to do their job. Long likens the approach to training sniffer dogs on a particular scent.
“When they get to work, they know what they’re searching for,” she said.
First approved in melanoma, these drugs have since been applied to cancers of the lung, kidney and other tissues, in many cases with great impact. But the melanomas that Scolyer and Long succeeded in treating have a high number of genetic mutations that alert T-cells to destroy the cancer. Mutation levels in glioblastomas usually aren’t as high.
The potential side effects are also threatening. If the therapy were to worsen brain swelling, it could be lethal, Long said.
‘Not Good Enough’
“If you’re facing potentially a lot of toxicity and you’re not sure if something is going to work, people shy away,” said Hussein Tawbi, who co-directs the brain metastases clinic at the University of Texas MD Anderson Cancer Center in Houston. “But if we don’t push it, those patients are not going to get better.”
Indeed, immunotherapy’s track record against glioblastoma has been poor, with a string of failed late-stage trials since 2012, including four involving immune checkpoint inhibitors from Opdivo-maker Bristol Myers Squibb Co. The negative results — and average costs of some $45 million for a late-stage cancer trial — have made drugmakers cautious about launching more large studies.
Bristol and Roche Holding AG are following Scolyer’s course, company officials said, adding that it’s too early to make research decisions based on a single patient’s treatment. Roche, maker of cancer blockbusters like Perjeta and Tecentriq, is running an early-stage trial of a novel antibody therapy for glioblastoma, and Novartis AG said it’s studying drugs that use radioactive particles to target the cancer in a number of early-stage trials.
Many studies of immunotherapy in glioblastoma haven’t chosen the patients most likely to benefit or identified the reasons for failure, according to Mustafa Khasraw, a brain cancer specialist at Duke University School of Medicine in Durham, North Carolina. He’s trying to correct that with detailed assessments of patient tissue samples before, during and after treatment.
“There is a problem in the field,” Khasraw said. “People don’t want to move beyond standard of care. We’ve been trying the same treatment for decades, and it’s just not good enough. Patients still die the same terrible death from this disease.”
Grim Diagnosis
It caught Scolyer unawares. A fitness fanatic, the lean, sandy-haired 56-year-old represented Australia at the World Triathlon Multisport Championships in Ibiza, Spain, in May. He was in southern Poland later that month lecturing on melanoma and relaxing in the Tatra Mountains with his wife, Katie, when the first signs of trouble emerged.
“We climbed up to see some incredible views and then the next day I was unwell,” Scolyer said in one of more than three dozen social media posts chronicling his four-month treatment journey. Hours later, barely conscious, he had a seizure.
An MRI scan at Krakow University Hospital found a mass on his temporal lobe. By the time the Scolyers rejoined their three teenage children in Sydney five days later, his collaborator Long was already formulating a treatment plan. On June 5, Scolyer underwent a craniotomy — a skull-opening procedure to obtain tissue — that showed just how aggressive his tumor was.
Doctors usually follow surgery with the chemo treatment for glioblastoma, temozolomide. But the tests indicated that Scolyer’s tumor would respond poorly to it.
There was another reason to skip temozolomide: the drug, along with steroids usually given for brain swelling, can impair immune activity and potentially sabotage the benefits of immunotherapy. Even Roger Stupp, the Northwestern University oncologist who pioneered temozolomide’s use in glioblastoma, thought it best to leapfrog the standard protocol.
“You cannot win a Formula 1 race with one foot on the gas pedal, and the other on the brakes,” Stupp said in an emailed response to questions about Scolyer’s case.
Four days after surgery, Scolyer received his first intravenous dose of a cocktail of drugs aimed at helping the immune system attack his tumor.
Muted Immunity
Twelve days later, surgeons made a 6-inch incision near Scolyer’s left temple and spent six hours removing a golf-ball-sized tumor from his brain. The surrounding tissue was doused in liquid immunotherapy drugs. The researchers turned their eyes on the tumor, looking for a surge in T-cells that would indicate the immune system was attacking it.
The drugs had crossed the blood-brain barrier, a vascular shield against toxins and infections that’s also been considered an obstacle to glioblastoma treatment. And under a microscope, the immunotherapies appeared to be impeding a protein on T-cells called PD-1, effectively releasing a brake so that the immune cells could better attack the cancer. Also, there were 10 times more cancer-fighting T-cells in the resected tumor after the infusion of the drug cocktail than in the pre-treatment biopsy.
Read More: mRNA Is Magic in Covid Vaccines. What Else Can It Do?
While that early evidence is promising, it’s too early to tell if the data will translate into clinical benefit. As a seasoned oncologist and scientist, Long said she was accustomed to treat such findings from a single patient with caution. But as Scolyer’s close friend and colleague, she views them as a source of optimism and pride.
“We could not have hoped for better results,” Long said. “We have generated in 10 weeks discoveries that would normally take many years.”
The researchers weren’t done firing on the tumor: After six weeks of daily radiation therapy, Scolyer then received a personalized cancer vaccine. Administered every two weeks, the shot is a collection of proteins that mimic features of his tumor, giving his immune system additional training to attack remnant cancer cells.
The Unbeatable
There have been setbacks. The first dose of immunotherapy brought on low-grade fevers, shivers, nausea, and an itchy rash that Scolyer called “manageable.” He also had abnormal liver tests in late June, which led Long to delay a second infusion and give only one immunotherapy drug. When things settled, he received more combination therapy without any liver problems. A routine follow-up scan on Sept. 29 found no recurrent tumor or treatment complications, he said.
Despite the side effects, he remains well enough to maintain an active lifestyle and marked the end of his radiation therapy with a 7 1/2 mile run.
Some brain cancer specialists caution against giving too much weight to results from a single patient. Whether or not the intervention works, the detailed case study will add to the understanding of immunotherapy’s potential in glioblastoma, and perhaps unleash new approaches.
“I may survive — I may beat the unbeatable — and, in doing so, will massively impact the whole brain cancer field,” Scolyer said. “At worst, I’ll leave a legacy of increased scientific knowledge to benefit future brain cancer patients.”
--With assistance from Nacha Cattan.